Written in consultation with McKinley Morrison, RN
It’s lonely, being a caregiver.
When your loved one has dementia, the loneliness can be especially profound.
That’s because the opposite of loneliness is connection. And how do you connect with someone who doesn’t share your reality? To someone who forgets what day it is and where they are? Who may even get confused about who you are?
How do you connect when you are you are mourning the person they used to be? Especially when that person is right in front of you, and yet at the same time isn’t?
You connect by embracing what is, and by learning to navigate within their world.
It’s a journey that turns heart-wrenching into beautiful and awful into meaningful. It will transform you in profound ways and leave your heart bigger, even though you thought it was breaking.
If you let it, that is.
Finding the beauty in this journey begins with the same principle that makes it all so difficult to begin with: connection. And at the heart of connection is empathy.
Why Empathy Matters
Empathy is your ability to understand and share the feelings of someone else.
In all of life, our ability to step outside our own worries, prejudices, and pain determines how successful our relationships will be.
Caring for someone with dementia is no different. It’s just way harder.
No only do you have to accept that this other person has a different perspective and feelings than you do, you have to accept that their brain is functioning so differently than yours that time and space have become fluid. That their sensory perceptions may be distorted. And most of all, that they physically lack the ability to meet you halfway and see things from your perspective.
And then you treat them with respect anyway.
Because inside, they are still a person. They feel when you listen with kindness. They feel when you value their concerns enough to engage with them on their terms. And they thrive when your empathy is so deep and unselfish and real that it forms a bridge between you, crossing over the confusion and unreal perceptions pushing you apart.
Your empathy has to become bigger and better than it’s ever been before.
How to Develop Bigger, Better Empathy
The first step in developing bigger, better empathy is reframing how you think of the confused person.
They aren’t a shell of a person.
They are person experiencing life differently.
Their reality is what it is because of how their brain is functioning. Your reality also is what it is because of how your brain is processing the world. Both filters are imperfect measures of objective reality.
You can’t see the full spectrum of light that a honeybee can, hear all the pitches a dog does, or sense bioelectric fields the way a shark can.
There are many different experiences of the same reality.
Accept that this person in front of you is a valuable human being. They are worthy of respect and kindness, regardless of their limitations.
I have been fascinated by the varying degrees of success different caregivers can have with the same patient.
Even when caregivers have all heard the same basic guidelines for helping confused patients, patients are still consistently peaceful and happy with some caregivers and agitated and aggressive with others.
The difference has a lot to do with the underlying attitude each caregiver brings to their interactions. It isn’t just the words they say, it is the degree of respect and kindness their body language and tone convey, and their patience and creativity in seeking to understand and respond to the patient’s perspective.
There are specific things you can do to communicate acceptance and respect.
What Caregivers Who are Good at Interacting with Dementia Patients Do Differently
Focus on what they can do instead of what they can’t:
Your attitude and the quality of your relationship will improve when you focus on abilities instead of limitations. Do you define them as a person who can’t remember recent events, or as a person with a rich history who can share stories from their childhood?
Look for their strengths:
Do you see a person as difficult or determined? Oppositional or strong? The more you frame their behavior in terms of strengths instead of weaknesses, the easier it will be to help them maximize their positive qualities.
Be in the moment:
Dementia patients can share beautiful moments of joy and connection with caregivers. Be present for those moments when they come instead of focusing on their impermanence.
Don’t talk down to them:
Most dementia patients notice and react badly when a caregiver seems condescending. Even a patient who is confused about other things can often read subtle body language and voice cues that signal they are being disregarded or their concerns aren’t taken seriously. This is a source of much conflict and frustration between patients and caregivers.
Validate their feelings:
Their beliefs about a situation may be inaccurate, but the emotions that result are real. Help them feel your genuine understanding and support.
Listen between the lines:
When you need to change a patient’s behavior, first ask yourself what the person is feeling. If you take time to validate their feelings, they will be more open to redirection or distraction.
Meet them in their reality:
Work within their frame of reference instead of arguing, even when their beliefs are inaccurate.
Try to accommodate their behavior when they can’t control it:
Find compromises that keep them safe and happy, even if they seem unconventional. Avoid power struggles.
Keep their sense of control intact:
Offer more than one choice whenever possible. Many dementia patients find direct “orders” threatening. However, too many choices can be frustrating and overwhelming. It often works best to offer a couple of clear, well-defined options.
View aggression as a form of communication:
You have to keep yourself safe, of course. But recognize that if a dementia patient lashes out, it often has meaning. As patients lose the ability to articulate their feelings in the ways they used to, they resort to other methods of communication. To de-escalate a situation, ask yourself, What is this person feeling? Respond to the emotion or need rather than to the behavior.
Build routines that avoid triggers:
Notice those things that are harder to deal with because of their condition. For example, some dementia patients have visual disturbances that make things like walking over entry mats frightening. Help them structure their lives to avoid these.
Make eye contact:
Connect to them one human being to another.
Recognize that the disease impacts different brain functions at different rates:
Dementia patients often lose abilities like filtering language and controlling impulses before they lose the ability to read the reactions of other people. That means they can seem childlike, and in one sense they are. They can’t control their own reactions as they used to. However, they can still read yours. If you treat them in a way that feels condescending, it will worsen the situation.
Help them to connect to themselves through the memories they still have:
Have the kindness to share music, smells foods, pictures, and activities that bring them back to themselves. Most dementia patients have intact memories from their earlier years long after they lose short term memories.
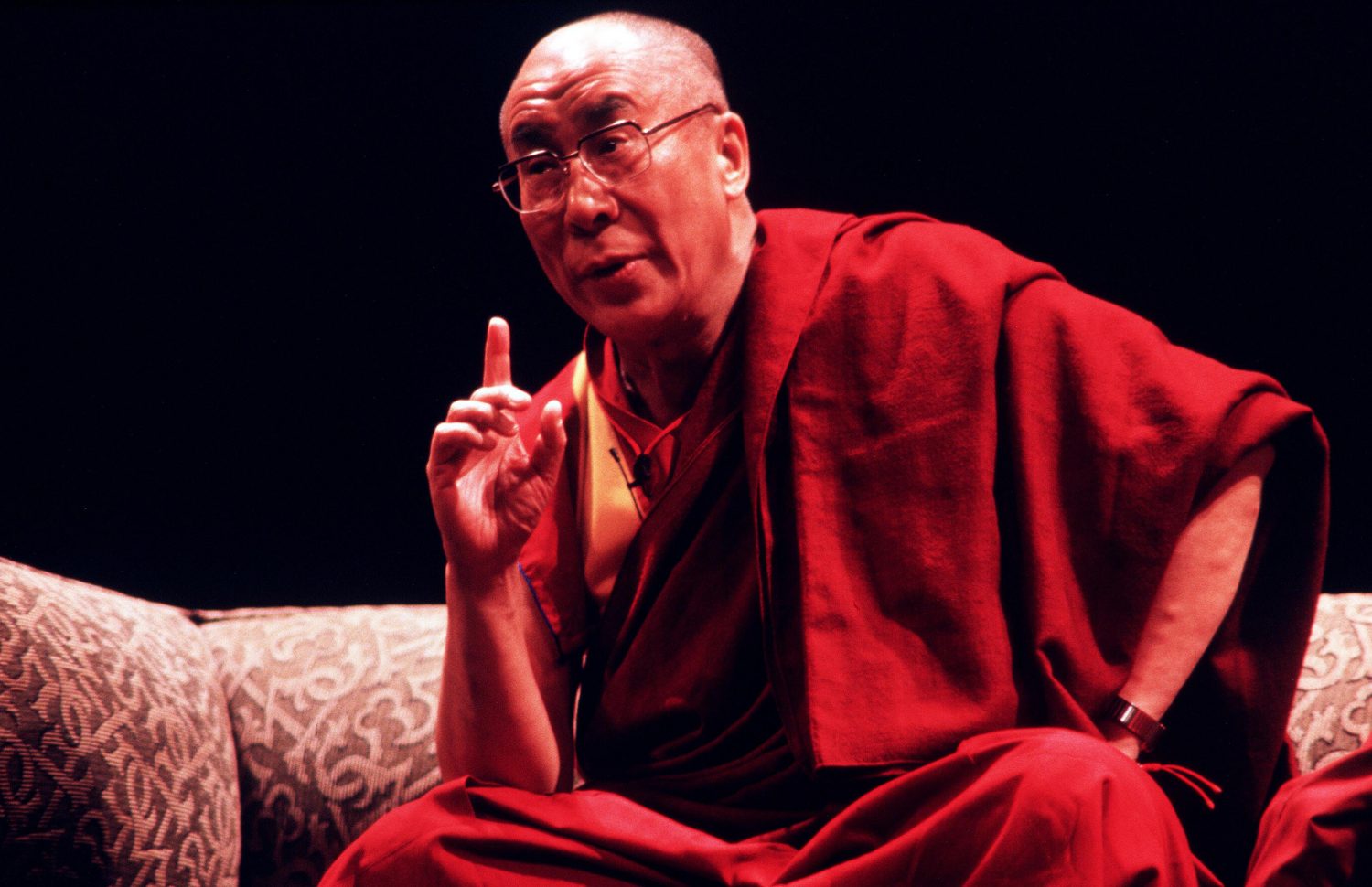
The medical community is just beginning to grasp the powerful potential of empathy to transform care for dementia patients. And the research emerging is exciting.
What the Medical Community is Learning About Empathy in Dementia Care
There is a growing awareness in the medical community that dementia patients have often been poorly cared for because they were poorly understood. For example, dementia patients who act out may be restrained or treated with antipsychotics, even though the root cause of their behavior is something like boredom or loneliness.
Restraints don’t cure bordeom or loneliness. Niether does medication. Relying on these interventions often escaltes difficult behavior even further.
Check out this case study, in which the frustrated staff at a long term care facility described the destructive nature of one of their Alzheimer’s patients to researcher Phillipe Voyer. The man ripped a sink off the wall and pulled tiles out of the floor with his bare hands.
Voyer immediately saw the man’s potential, describing him as focused, strong and determined. Then he used empathy to try to investigate the root cause of his behavior. He explains,
Some residents who have dementia may have worked all their lives doing manual labourer, for example. . . When they feel bored, they go back to doing what they know. We learned that the gentleman who tore the sink off the wall and the tiles from the floor had been employed in home construction. He was just doing what he knew how to do. Likewise, people who are bored may start to explore. They go into other people’s bedrooms. When they do, they get involved in altercations with other residents. Soon they are labelled as having behavioural issues. What do we do then? We medicate them. It’s as simple as that.
Using bigger, better empathy allows you find new ways of understanding what your loved one really needs. You can avoid overmedication and improve quality of life for your loved one.
What Bigger Better Empathy Looks Like
In carrying for someone who is confused, empathy means keeping them safe while navigating the world on their terms.
What do you do if Grandpa is agitated at 3am because he can’t find his clothes and briefcase, and he thinks he’s going to miss a meeting at work?
Don’t try to explain that he retired over twenty years ago, all those items have long since been discarded, and he doesn’t have a job. He will be more frightened, more confused, and more combative.
Instead, work within his frame of reference. You might say, “You have plenty of time. Look out the window. See how it’s still dark outside? You probably woke up early because you were thinking about your meeting. But you need to sleep so you can be rested for work.”
What do you do if Grandma is restless and anxious, searching the house for her husband?
Don’t tell her he died 15 years ago. She will either not believe you, or she suffer through the shock and pain of his death as if learning about it for the first time. Suggest that maybe he had to leave for a while, and give her a familiar task, like folding (and refolding) towels that she remembers doing while waiting for him in the past.
You may not be speaking objective reality, but you are speaking to their reality.
Yes, you’ll have the same conversation, or a similar one, many times. Looking at the situation without empathy, it can feel pointless and discouraging because you will never change their perspective in a lasting way.
But what if that isn’t the goal?
What if the goal of each of those repetitive conversations is to bring comfort and safety to someone who is struggling? And what if each time you do that, you are succeeding?
Every time you interact from a place of empathy, your loved one experiences their worries being heard and their fears being calmed.
And that is one of the core experiences that brings happiness in every stage of life.
What Empathy Has to Do with You
There’s a bonus to all this talk about empathy.
When you open your heart to provide more connection and better care to your loved one, you also open yourself to comfort and healing.
Check out this community of Alzheimer’s caregivers who are learning how to find joy instead of suffering in their caregiving experience.
They are replacing grief and discouragement with hope and happiness as they change the ways they view and interact with their loved one. You can too.
As you discover ways to understand and connect to your loved one, you will gain priceless moments with them, and you will learn to recognize compassion, joy, love, tenderness, and gratitude in your own experience.
Caregiving is a challenging journey. But it can also be a journey of meaning and connection, for both you and for your loved one.





























4 thoughts on “When Caring for a Loved One with Dementia: How to Help Them (and Also Help Yourself!)”
This article was most informative. I wish I had this information when I was dealing with my Mother who had been diagnosed with Dementia several years ago. I was here care giver for 2 years before she got admitted to a nursing facility. Very draining for the whole family, especially for me!
Thank you for reaching out. Caregiving is such demanding work. You have much to be proud of for your years of service to your mom.
When I read all this article I was cried a lot because I take care of my mother and she died 5 months ago. I was looking after her and I tried to understand all this process of dementia but was very sad and painful and have lots of stress. Anyone of any institution help me to explain me this process of get all this information and I felt very guilty when sometimes I have had depression and I can’t cope with her dementia. I said how late I know now all this process. I read that because I friend share at Facebook.
You did a beautiful thing caring for your mother, especially doing it without the support and education that could have helped. Please take comfort in knowing how your honored her and showed your love. Caregiving is hard work.